WELI Advisors
 Rita Agarwal, MD
Rita Agarwal, MD
I did my training at Baylor College of Medicine and University of Colorado and spent over 20 years at the Children’s Hospital of Colorado, where I was the Pediatric Anesthesia Fellowship Director for 17 years, Director of the Acute Pain Service for 5 and Director of Pediatric Education. I am the Chair of the Pediatric Anesthesia Education Committee, the Chair of Clinical Competence Committee at Stanford, and serve on the Stanford Pediatric Anesthesia Leadership Committee.
I have served on the Society for Pediatric Anesthesia Board of Directors for many years in a variety of roles, including Communication Chair, Newsletter Editor, and At-Large Board Member. I am the past Chair of the American Academy of Pediatric Section on Anesthesiology and Pain Medicine and currently the President of the Society of Pediatric Pain Medicine (2019-present). My most unexpected experiences have occurred as a result of my involvement with the California Society of Anesthesiology, that have led to participation in advocacy, testifying in the California Assembly and interaction with a much wider group of physicians, health care professionals and other people on a variety of topics.
I have 3 boys (twin teenagers and one college aged ) a dog and now 4 cats (we just found and adopted a kitten in November.
My passion is education, mentorship, sponsorship, and advocacy (for everyone). My mottos are “It will be an adventure” and “we are all in this together”
 Aditee Ambardekar, MD
Aditee Ambardekar, MD
Dr. Aditee Ambardekar is an Associate Professor and Distinguished Teaching Professor at UT Southwestern Medical Center, Department of Anesthesiology and Pain Management. She received her medical degree from the University of Maryland School of Medicine in Baltimore, Maryland. She later completed her Anesthesiology Residency and Pediatric Anesthesiology Fellowship at the Hospital of the University of Pennsylvania and The Children’s Hospital of Philadelphia, respectively. She joined the faculty at UPENN/CHOP and quickly got involved in fellowship education and administration and simulation-based education. During her nearly 5 years at CHOP, she helped to develop the departmental simulation program and helped run the fellowship program. She also earned her Master’s in Education from the Graduate School of Education at the University of Pennsylvania. She joined the faculty at UT Southwestern Medical Center and Children’s Medical Center in Dallas in 2014, where she now serves as the Residency Program Director for Anesthesiology. Other local and national responsibilities include Simulation Educator at the departmental and institutional level, ABA Applied Examiner, and most recently the Chair of the Anesthesiology Review Committee at the Accreditation Council for Graduate Medical Education (ACGME). She spends the majority of her clinical responsibility as the pediatric anesthesiologist at the Parkland Burn Center. She has recently published in the burn literature, simulation literature, and medical education literature as it pertains to undergraduate and graduate medical education.
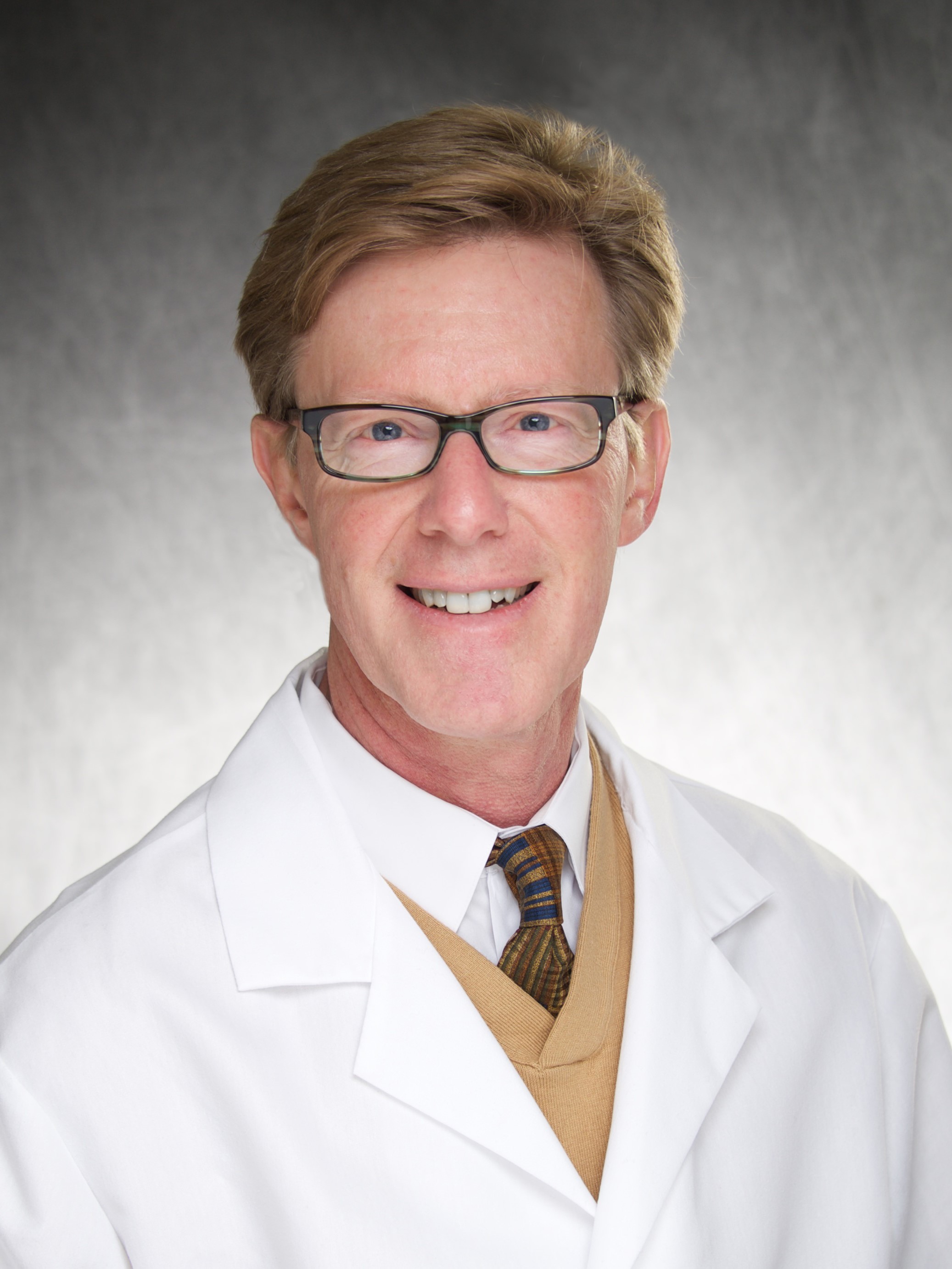
 Corrie Anderson, MD, FAAP
Corrie Anderson, MD, FAAP
Dr. Corrie T.M Anderson is a Professor of Anesthesiology and an Adjunct Professor of Pediatrics at the University of Washington school of Medicine. Professor Anderson is a Board Certified Anesthesiologist with a Certificate of Added Qualification in Pain Management. He is also the Director of theCenter at Seattle Children’s Hospital and Regional Medical Center.
Born in Minneapolis, Minnesota, Dr. Anderson attended Harvard University and graduated with honors from the department of Biochemistry and Molecular Biology. He spent six years at Stanford University Medical School in the Medical Scientist Training Program where he did graduate work in DNA repair while obtaining his MD. Following Stanford, Dr. Anderson traveled back to Massachusetts to Boston Children’s Hospital where he completed an internship and residency. He was enticed by the anesthesiology field and subsequently decided to take up anesthesiology and complete an anesthesiology residency at Boston’s Brigham and Women’s Hospital. After Dr. Anderson’s residency, he returned to Boston Children’s’ Hospital for a Pediatric Anesthesiology fellowship.
During his fellowship, Dr. Anderson met and worked with physicians; Dr. Charles Berde and Dr. Navil Sethna, where he became increasingly interested in Pediatric Pain Management. Amidst newfound fatherhood due to the birth of his first child in 1988, Dr. Anderson moved again, across the country to UCLA and established the second Pediatric Pain Management Service on the West Coast.
In 1989 Dr. Anderson began to build a multidisciplinary pain program that provided consultative patient care for pediatric patients who had acute or chronic pain problems. In addition to being the Director of the UCLA Pain Management Program, Dr. Anderson became Director of Pediatric Anesthesiology at the UCLA School of Medicine in 1990. He was actively involved in teaching pain management and anesthesiology to undergraduates, medical students, residents, fellows, nurses and other staff, winning several teaching awards in the process.
After 13 years at UCLA and becoming a Professor of Anesthesiology and a Professor of Pediatrics, Dr. Anderson was recruited to Seattle Children’s Hospital and Regional Medical Center to become its Director of the Pain Medicine Program. Dr. Anderson has lectured nationally and internationally on pediatric pain and pediatric regional anesthesiology. He holds both an American and European patent on a force warm air blanket, the “Corrie Cover”. Dr. Anderson was awarded the Golden Apple Seed teaching award three times by the University of Washington anesthesiology residents and named one of Seattle’s best doctors in Seattle Magazine for more than 10 consecutive years. He was elected to the Association of University Anesthesiologists and his most recent focus has been in the development of an ultrasound guided pediatric regional anesthesiology curriculum. He is currently the Director of the Seattle Children’s Hospital Center for Excellence in Pediatric Regional Anesthesiology. In 2015 Dr. Anderson and his wife started the “Dr. Corrie T. M. Anderson and Virginia E. Williams II Regional Anesthesiology Research and Education Endowment in the Department of Anesthesiology and Pain Medicine at the University of Washington School of Medicine.
Dr. Anderson is proud to have raised with his wife Virginia, a daughter and son whom have graduated from Harvard and MIT respectively. Both children work in healthcare.
Outside interested include: photography, tennis, travel, skiing and inventing.
 Carolyn Bannister, MD
Carolyn Bannister, MD
Dr. Carolyn Bannister, Mayo Clinic Jacksonville, is Chair of Pediatric Anesthesiology and Critical Care Medicine at Nemours Children’s Specialty Care and Wolfson Children’s Hospital in Jacksonville, Florida. She completed her medical training at Duke University School of Medicine and her Pediatric/Internal Medicine and Anesthesiology residencies at Emory University School of Medicine. She remained on faculty at Emory University following her training and was the Chief of Pediatric Anesthesiology at Emory for 17 years. During that time she was Program Director for the Emory Pediatric Anesthesiology fellowship.
She served as President of the Pediatric Anesthesiology Program Directors’ Association for two years. She was Chair of the AAP Section on Anesthesiology and Pain Medicine for two years.
She assumed the Chair of Pediatric Anesthesiology and relocated to Jacksonville, Florida in January 2015.
 Karen Bender, MD
Karen Bender, MD
Dr. Karen Bender is the Division Chief of Cardiac Anesthesiology at the Nemours Children’s Hospital in Orlando, Florida. She attended college and medical school at the University of Florida in their Junior Honors Accelerated Medical Program followed by residencies in pediatrics and anesthesiology including a pediatric anesthesia fellowship at the Johns Hopkins Hospital. After two years on faculty at Johns Hopkins, she returned to Florida in first a private practice setting then as part of the Nemours Children’s Clinic caring for patients at the Arnold Palmer Hospital for Children. While at Arnold Palmer Hospital, she helped build a strong team of pediatric anesthesiologists and CRNA’s, helped train residents from the University of Florida and SRNA’s from Barry University while serving in many roles including Chairman of Anesthesiology. After raising her three children, Dr. Bender moved back to her birthplace, Philadelphia, to pursue her passion for teaching and mentoring at the Children’s Hospital of Philadelphia in the Division of Cardiothoracic Anesthesiology before returning to Florida to rejoin Nemours and help develop a new cardiac program in Orlando. Karen enjoys spending time with her family and friends, international medical missions, caring for patients with congenital heart disease, kayaking, teaching and investing in others.
 Tarun Bhalla, MD, MBA, FAAP
Tarun Bhalla, MD, MBA, FAAP
Dr. Bhalla currently serves as Chairman of the Department of Anesthesiology and Pain Medicine at Akron Children’s Hospital. He recently transitioned from Nationwide Children’s Hospital where he served as Vice Chairman of Comprehensive Pain Services, Director of the Pediatric Regional Anesthesia Fellowship, and Associate Professor of Anesthesiology at The Ohio State Wexner Medical Center. Dr. Bhalla serves a Board of Director position on the Society of Pediatric Anesthesia, as well as will be the upcoming Program Chair for the Annual Meeting in 2020. He has provided lectures and workshops both nationally and internationally over the past decade, and has multiple peer reviewed publications and book chapters. Dr. Bhalla serves as both a mentor and advisor to a wide variety of mentees. He enjoys engaging on emotional intelligence, situational awareness, conflict resolution as well as self empowerment and leadership delegation. He looks forward to being an active member of WELI.
 Anne Boat, MD
Anne Boat, MD
Anne C. Boat, MD, is the Associate Chief Medical Officer and Director of Fetal Anesthesia at Ann & Robert H. Lurie Children’s Hospital of Chicago. She is also an Associate Professor of Anesthesiology at Northwestern Feinberg School of Medicine in Chicago, Illinois. Dr. Boat received an M.D. from the University of North Carolina School of Medicine and completed an anesthesia residency and a pediatric anesthesia fellowship at the University of Cincinnati College of Medicine and Cincinnati Children’s Hospital Medical Center, respectively. In addition to her role as Director of Fetal Anesthesia for the Cincinnati Fetal Center, Dr. Boat served as the Chief Patient Experience Officer and leader of the Center for Patient/Family Experience (PFE) at Cincinnati Children’s Hospital Medical Center (CCHMC) from 2013-2018. In this role, she sought to translate patient/family understanding into system-wide improvement and innovation priorities. In July 2018, Dr. Boat joined the Ann & Robert H. Lurie Children’s Hospital of Chicago as the Associate Chief Medical Officer. Her focus is on the Medical Staff/Provider Services and, more specifically, provider engagement and well-being. Through her role as Director of Fetal Anesthesia, Dr. Boat has worked on numerous quality improvement projects in the operating room setting related to safety, efficiency and improved communication across multidisciplinary teams.
 Tanna J. Boyer, DO, MS, FASA
Tanna J. Boyer, DO, MS, FASA
Tanna Boyer is an Associate Professor of Clinical Anesthesia at Indiana University School of Medicine, working clinically as a pediatric anesthesiologist at Riley Hospital for Children since 2017. Prior to this she worked at the Medical College of Georgia. Dr. Boyer went to medical school at the Philadelphia College of Osteopathic Medicine and completed her medical training at Temple University for anesthesia residency, and the Children’s Hospital of Philadelphia for fellowship. While at MCG, she completed a Medical Education Research Fellowship with the Educational Innovation Institute and participated in the AAMC Leadership Education and Development (LEAD) program. She introduces herself as a “physician mom, medical educator, and patient advocate”.
Dr. Boyer recently completed the Health Innovation and Implementation Science Graduate Certificate through CHIIS at IUSM and is interested in using what she has learned to improve medical education and healthcare. She has worked in academic medicine her entire career and served as Lead Career Advisor for medical students applying to residency programs in anesthesiology at both the Medical College of Georgia and Indiana University. She has taught and directed UME electives in anesthesiology, mentored anesthesiology residents as cohorts and as individuals, served as liaison for two Anesthesiology Student Interest Groups, participated in residency interviews, participated in the Penn State University Internship program with undergraduate students, and served as Director of Simulation. She enjoys spending time helping students and trainees make life decisions and watching them grow and develop.
Dr. Boyer is a life-long learner committed to improving medical education and advocating for safe patient care and the practice of anesthesiology. As an advocate for the specialty, she serves on the Indiana Society of Anesthesiologists Board of Directors and as ISA Education Committee Chair. She is also a member of two ASA committees and has been a delegate or alternate delegate to the ASA HOD since 2018.
 Debnath Chatterjee, MD, FAAP
Debnath Chatterjee, MD, FAAP
Dr. Debnath (Dabe) Chatterjee is a pediatric anesthesiologist at Children’s Hospital Colorado and an Associate Professor of Anesthesiology at the University of Colorado. After completing medical school in India, he moved to the United States to complete an anesthesiology residency at SUNY Upstate Medical University in Syracuse followed by a pediatric anesthesiology fellowship at Boston Children’s Hospital. As the program director of the pediatric anesthesiology fellowship at the University of Colorado, he enjoys mentoring and supporting the next generation of leaders in the pediatric anesthesia community. He is very excited to be a part of the WELI program. His areas of clinical interest include anesthesia for fetal interventions, and he is the Director of the Fetal Anesthesia program at the Colorado Fetal Care Center. He is an Executive Committee member of AAP’s Section on Anesthesiology and Pain Medicine and represents them at the National Button Battery Task Force. He is also an active member of SPA’s Education Committee, Communications Committee and ASA’s Committee on Pediatric Anesthesia. He is an oral board examiner for the American Board of Anesthesiology. Dr. Chatterjee is a strong believer in e-learning and is one of the Pediatric Anesthesia Section Editors of Open Anesthesia that records monthly videocasts, ask-the-expert interviews and virtual grand rounds. He is married to his wife, Piyali and they have two children, Rohan and Riya.
 Vidya Chidambaran, MD, MS
Vidya Chidambaran, MD, MS
I am an Associate Professor of anesthesia at Cincinnati Children’s Hospital Medical center. I am also the director of perioperative pain which is well aligned with my academic and research goals. I believe every individual is unique. So, whether it is anesthesia and pain management for patients or career advancement plans for colleagues, one size does not fit all. Individualized and tailored plans and opportunities need to be formulated for individual fulfilment. My career has been focused on research in genomics and psychological aspects of chronic post-surgical pain in children, and thus far has resulted in several funding awards and publications. I am also involved with several collaborative projects with our surgical colleagues including design thinking projects, and development of ERAS protocols and key performance indicators to improve the pain experience in children. I am on the board of directors of the SPPM, and have been co-chair/actively participate on committees in the American pain society and International association for the study of pain. I have benefitted immensely from the mentoring and training I received during my Translational Scholar Career Awards in Pharmacogenomics and Personalized Medicine (K23) award from the NIH, and recently received R01 level funding from NIAMS. I am keen to pass on the blessings I have received and help advise junior colleagues in any capacity that I can. I have participated in several leadership and women-to-women mentoring panels/workshops to prepare me for this. I am looking forward to embarking on a mutually satisfying and self-realizing journey with mentees, sharing and learning along the way. One of my favorite quotes is “For success, like happiness, cannot be pursued; it must ensue, and it only does so as the unintended side effect of one’s personal dedication to a cause greater than oneself…” – Viktor E Frankl.
 Franklyn Cladis, MDD
Franklyn Cladis, MDD
Franklyn Cladis is an Associate Professor of Anesthesiology at The UPMC Children’s Hospital of Pittsburgh. He trained in both internal medicine and anesthesiology at the University of Rochester School of Medicine. His Pediatric Anesthesiology fellowship was completed at The Children’s Hospital of Boston. He is board certified in Internal Medicine, Anesthesiology, and Pediatric Anesthesiology. Dr Cladis provides anesthesia care for infants and children in the operating room, on the pediatric pain service, and the pediatric liver transplant team. Areas of clinical interest include the anesthesia care of children having craniofacial surgery, pediatric perioperative pain, point-of-care ultrasonography and education. He is an editor for Smith’s Anesthesia for Infants and Children for the 8th and 9th edition and is currently working on the 10th edition. From an educational perspective, Dr Cladis has been the program director for the Pediatric Anesthesiology Fellowship since 2007. He is also one of the coordinators for the annual faculty development workshop in the division of Pediatric Anesthesiology in Pittsburgh. He is a Full examiner for the American Board of Anesthesiology (ABA) Applied Exam and is Vice Chair of the ABA Pediatric Anesthesiology exam committee. He has been a member of the Pediatric Anesthesia Program Directors Association (PAPDA) since 2010 and is currently President of this organization.
 Joseph Cravero, MD, FAAP
Joseph Cravero, MD, FAAP
Joseph Cravero MD FAAP is a Senior Clinical Associate at Boston Children’s Hospital and Associate Professor of Anesthesiology for Harvard Medical School. He currently serves as the Chief of Pain Medicine for the Department of Anesthesiology, Critical Care, and Pain Medicine. His career has been dedicated to optimizing the care of children through clinical care and research work involving sedation, pain control, and operative outcomes. He has served as the Chair of the Section on Anesthesiology and Pain Medicine for the American Academy of Pediatrics and has served on the Board of Directors for the Society for Pediatric Anesthesia. He was the founder and past president of the Pediatric Sedation Research Consortium and the Society for Pediatric Sedation. His current work is focused on mentoring pediatric anesthesia fellows and staff on the use of large data sets to optimize pain management and operative outcomes nationally and at Boston Children’s Hospital.
 Priti Dalal, MD, FRCA
Priti Dalal, MD, FRCA
Dr. Priti Dalal is a Pediatric Anesthesiologist at the Penn State Health Department of Anesthesiology and Peri-operative Medicine, Division of Pediatric Anesthesia, Penn State Health Children’s Hospital, Hershey, PA. She is Division Chief for Pediatric Anesthesia and Vice-Chair for Faculty Development and Public Affairs. Dr Dalal holds the academic rank of Professor of Anesthesiology at Penn State College of Medicine. She is actively involved with pediatric anesthesia quality at her institutional level and at the SPA. Her research interests include pediatric airway and pediatric pain assessment. Throughout her career, she has had wonderful advisors and mentors, internally and externally especially at the SPA. She firmly believes that good advising and mentoring contribute significantly to the success of an individual. She is committed to development of careers of faculty. She is actively involved with mentoring medical student, residents and faculty in her department and is very enthusiastic to be a WELI advisor
 Peter J. Davis, MD
Peter J. Davis, MD
Dr. Peter J. Davis is a Professor of Anesthesia and Pediatrics at the University of Pittsburgh School of Medicine and Anesthesiologist-in-Chief at the Children’s Hospital of Pittsburgh. Following graduation from the Albert Einstein College of Medicine, Dr. Davis completed his pediatric residency and chief residency at the University of California San Francisco and his anesthesia residency at the Massachusetts General Hospital. Dr. Davis also completed a 1year fellowship in pediatric critical care and pediatric anesthesia at the Children’s Hospital of Philadelphia. Dr. Davis is board certified in pediatrics and anesthesiology and has subspecialty certification in Pediatric Anesthesiology. He was the Pediatric Section Editor of the journal Anesthesia & Analgesia from 2004 till June of 2014 and currently is Senior editor for the journal. Dr. Davis is also the editor of the anesthesia textbook “Smith’s Anesthesia for Infants and Children.” Dr. Davis has over 95 peer reviewed articles and over 60 book chapters. His career has been devoted to the perioperative care of children and his research interests have focused on anesthetic drug pharmacology in children and neonates. He holds the Joseph H. Marcy endowed chair in Pediatric Anesthesiology at the UPMC Children’s Hospital of Pittsburgh.
 Nina Deutsch, MD
Nina Deutsch, MD
Dr. Nina Deutsch is Associate Professor of Anesthesiology and Director of Cardiac Anesthesiology at Children’s National Hospital in Washington, DC. She also serves as Vice-Chief of Academic Affairs for the Division of Anesthesiology, Pain and Perioperative Medicine. She has been successful in both clinical and education-based research throughout her career. In addition to this, she greatly enjoys working with and mentoring junior faculty in both research and educational projects, and she has implemented a faculty development program within her division. Nationally, Dr. Deutsch is the current President Elect of the Society for Pediatric Anesthesia. Involved with WELI since its inception as Co-Chair, she has watched WELI grow into a thriving community for women in pediatric anesthesiology and is dedicated to expanding its resources and endeavors in the future. She is married to her husband Andrew and has two children, Alex and Olivia.
 Laura K. Berenstain, MD
Laura K. Berenstain, MD
I have been a pediatric cardiac anesthesiologist since 1989, initially in private practice, followed by academic practice at Texas Children’s Hospital and The Children’s Hospital of Philadelphia. I am currently a member of the Division of Cardiac Anesthesiology at Cincinnati Children’s Hospital Medical Center, and I have just experienced two of the most exciting years of my career! After years of teaching trainees and colleagues how to care for patients with congenital heart disease I thought…Why not write a book about cardiac care OUTSIDE the cardiac OR? No one has done that. And so, as the year ends, I am watching that dream come to life as the chapters flow in and I happily edit. With luck by the end of 2020 there will be a book to hold in my hands: Congenital Cardiac Anesthesia: A Practical Approach. In addition to practicing pediatric cardiac anesthesia, my other major interests are physician wellness and resiliency, and mentoring, particularly for women. Having the opportunity to be part of the Steering Committee member for the Women’s Empowerment Leadership Initiative (WELI) and watching this amazing endeavor come to life has been invigorating, exciting and a privilege. I have enjoyed learning to add advising skills to my mentoring. Since I firmly believe that we can benefit from advising/mentoring at all stages of our career, I jumped at the chance to be both a WELI advisor and mentee this year. My WELI advisor was instrumental in helping me to define my goals and strategize my plan for the year, with the result that I was promoted to Clinical Professor of Anesthesiology in September. We have decided that the first year was such a success that we will continue in a mentor-advisor/mentee relationship for the coming year as well.
Having taught Mind-Body Seminars and created a Wellness Curriculum for our pediatric anesthesia fellows this year I look forward to taking a leadership role in our department in the coming year as we continue to expand our efforts to promote wellness and resiliency. WELI has already provided me with terrific networking opportunities to learn more about wellness initiatives at other institutions, and my next challenge to look forward to will be creating and sustaining a program for our department and institution.
 Elizabeth T. Drum, MD, FAAP, FCPP, FASA
Elizabeth T. Drum, MD, FAAP, FCPP, FASA
Elizabeth T. Drum, MD, FAAP, FCPP, FASA is an Associate Professor of Clinical Anesthesiology and Critical Care Medicine at the Perelman School of Medicine, University of Pennsylvania. Her clinical work is at the Children’s Hospital of Philadelphia where she serves as Medical Director of Radiology Anesthesia Sedation Services and Associate Division Chief for Clinical Operations. She also serves as the department’s Medical Director of Global Health Initiatives. Dr. Drum is chair of the American Society of Anesthesiologists (ASA) Global Humanitarian Outreach (GHO) Committee, a member of the Board of Directors of the ASA Charitable Foundation, a member of Council of the World Federation of Societies of Anaesthesiologists, a member of the Society for Pediatric Anesthesia Committee on Global Health, a member of the Board of Directors of the Alliance for Surgery and Anesthesia Presence, a member of the Global Initiative for Children’s Surgery, and was Chair of the Anesthesiology Investigative Task Force of the Pan-African Academy of Christian Surgeons.
Dr. Drum is a graduate of the University of Virginia and the Lewis Katz School of Medicine at Temple University. She completed Anesthesiology residency at Temple, Pediatric Anesthesiology training at St. Christopher’s Hospital for Children and served as a Major in the US Army Medical Corp. Dr. Drum was a full-time faculty member at Temple for 15 years where she was Professor of Anesthesiology and Pediatrics, Chair of the Medical Executive Committee, President of the Medical Staff and Chief Medical Officer of Temple University Children’s Medical Center, a member of the medical school admissions committee and held several other leadership roles at the University and the School of Medicine.
Dr. Drum founded the Resident International Anesthesia Scholarship program within the ASA GHO committee which has sent over 60 US anesthesiology residents to low resource settings to participate in educational outreach. She received the 2015 International Physician of the Year Award by medicalmissions.org and the 2020 Nicholas M. Greene, MD Outstanding Humanitarian Contribution Award from the American Society of Anesthesiologists for her work.
 Jim Fehr, MD
Jim Fehr, MD
Until June 2019, I was a Professor of Anesthesiology and Pediatrics at Washington University where I provided care for children at St. Louis Children’s Hospital in the cardiac OR and in the pediatric Cardiac ICU. Working with these patients required interdisciplinary discussions and diplomatic communication skills to help resolve conflict in difficult situations. It also has required mastery of end of life counseling for families of dying children. Since 2009, I was the medical director of the Pediatric Simulation Center at St Louis Children’s Hospital and have extensive experience in the use of simulation as an educational modality for skills training and to improve communication skills of providers. In 2014, was elected to the Board of Directors of the Society for Pediatric Anesthesia (SPA); in 2019 when I was appointed as Secretary Treasurer of the SPA. In 2023 I will begin a 2-year term as President of the SPA. In 2016 I was appointed Assistant Ombuds for the Washington University School of Medicine which required troubleshooting conflicts for medical school faculty. In August 2019 I became the Anesthesiologist-in-Chief at Stanford University’s Lucile Packard Children’s Hospital.
 John Fiadjoe, MD
John Fiadjoe, MD
Dr. Fiadjoe is an Associate Professor of Anesthesiology & Critical Care at the Children’s Hospital of Philadelphia and the University of Pennsylvania Perelman School of Medicine. He is dedicated to advancing patient care by investing in and developing clinical, research and education teams, mentoring and advising individuals to be their best possible selves and encouraging and facilitating collaboration and cooperation across diverse institutions to help advance pediatric care.
Dr. Fiadjoe’s leadership values include life-long learning, empathy, and grit. His favorite quote is by the author Simon Sinek “What good is having a belly if there is no fire in it. Wake up, drink your passion, light a match and get to work”
 Randall P. Flick, MD, MPH, FAAP
Randall P. Flick, MD, MPH, FAAP
Randall Flick, M.D., M.P.H., is a consultant in the Department of Anesthesiology with a joint appointment in the Department of Pediatric and Adolescent Medicine. Dr. Flick is Medical Director of the Mayo Clinic Children’s Center and in his role oversees all pediatric activity across the Mayo Clinic Enterprise reporting directly to both the Mayo Clinic Dean for Practice and the CEO. He holds the academic rank of Professor of Anesthesiology and Professor of Pediatrics. Dr. Flick received the R.N. diploma from St. Luke’s Hospital School of Nursing and the B.A. degree in biology from Moorhead State University. He earned the M.D. degree from the University of North Dakota School of Medicine (AOA) and the M.P.H. degree from The Johns Hopkins Bloomberg School of Public Health. Dr. He is holds board certification in four specialities including pediatrics and pediatric critical care (ABP) as well as anesthesiology and pediatric anesthesiology (ABA). He is past president the Society for Pediatric Anesthesia Board of Directors and for the United States Food and Drug Administration,served as Chair of the Advisory Committee on Anesthetics and Analgesic Drug Products and as a member of the Pediatric Advisory Committee. His research interests include outcomes in pediatric anesthesia, neurodevelopment effect of anesthetic exposure. Dr. Flick has an extensive track record of mentorship. Serving as advisor and mentor to many anesthesia residents, fellows and junior faculty at Mayo Clinic. In addition he for many years has mentored young members of the Society for Pediatric Anesthesia and young anesthesiologists from around the world including Colombia, South Korea and China. Dr. Flick and his wife Loree have three sons Bryant (Sara), Garrett (Tori), Grant (Emily) and a grandson (Owen).
 Susan M. Goobie, MD, FRCPC
Susan M. Goobie, MD, FRCPC
Specialty: Patient Blood Management, blood conservation methods, coagulation disorders, anti-fibrinolytics, anemia. Patient blood management quality improvement and clinical research, pharmacokinetic research.
Brief Resume:
- Anesthesia & Analgesia, Executive Section Editor
- Pediatric Anesthesia, Executive Editor
- Canadian Pediatric Anesthesia Society, Scientific Committee Chair
- Society of Pediatric Anesthesia, Patient Blood Management SIG Chair
- American Society of Anesthesia, Patient Blood Management , Research, and Pediatric committees member
- International Anesthesia Research Society, American Society of Anesthesia and Canadian Anesthesia Society, research committee member
- Society for the Advancement of Blood Management, past board member and chair of scientific committee and educational committee member
- Founder and director of the Dept of Anesthesiology @Boston Children’s Hospital Patient Blood Management Program
- Chair of Main Operating Room Research, Dept of Anesthesiology, Boston Children’s Hospital
- Founder and past director of Boston Children’s Hospital Pharmacokinetics Laboratory
- She is from Newfoundland, Canada and lives in Boston, MA, USA with her husband, 3 children and a golden retriever. She is an avid cyclist, skier and loves the outdoors.
 Jennifer K. Hansen, MD
Jennifer K. Hansen, MD
Jennifer K. Hansen, MD, is a Pediatric Anesthesiologist and Associate Professor of Anesthesiology at the University of Kansas, Kansas City. She completed her anesthesiology residency at the Cleveland Clinic and pediatric anesthesia fellowship at Children’s Hospital Colorado, University of Colorado. She has been at the University of Kansas since 2012, and currently serves as the Division Chief of Pediatric Anesthesiology at the University of Kansas Medical Center. Her professional interests include mentoring junior faculty, residents, and medical students, and international outreach through medical missions and education. She joined the WELI group as a mentor in the fall of 2019. Clinical and research interests include pediatric craniofacial surgery, neonatal perioperative hypothermia prevention, pediatric sedation practices in remote locations, and anesthesia for pediatric neuro-interventional radiology. Academic interests include being a facilitator for medical student education, resident education through simulation, OSCE board exam preparation for residents, OR team training for crisis management and intraoperative code blue training. She is married, with five adult children and twelve beautiful grandchildren.
 Zena Leah Harris, MD
Zena Leah Harris, MD
Z. Leah Harris, MD, is Chief of the Division of Critical Care Medicine at Ann & Robert H. Lurie Children’s Hospital of Chicago, and a Professor of Pediatrics in the Division of Critical Care Medicine at Northwestern University Feinberg School of Medicine. Her special areas of interest include transition metal biology, nutrition, medical education and inter-professional development.
 Stephen Hays, MD
Stephen Hays, MD
 Eugenie S. Heitmiller, MD, FAAP
Eugenie S. Heitmiller, MD, FAAP
Dr. Genie Heitmiller is the Joseph E. Robert, Jr. Professor and Chief of Anesthesiology, Pain and Perioperative Medicine at Children’s National Hospital in Washington, DC. She joined Children’s National in 2015 after 35 years at Johns Hopkins, where she completed her residency training in Pediatrics and Anesthesiology as well as fellowships in cardiac and pediatric anesthesiology, then served as faculty in the Departments of Anesthesia, Critical Care Medicine, and Pediatrics with expertise in pediatric cardiac anesthesia. She was Professor and Vice Chair for Clinical Affairs in the Department of Anesthesiology and Critical Care medicine at Johns Hopkins School of Medicine prior to accepting the position at Children’s National. Dr. Heitmiller has contributed to the field of anesthesia in numerous ways. She has authored or co-authored over ninety publications, including peer-reviewed manuscripts, invited publications, book chapters and an anesthesia handbook. She was on the leading edge of the national health quality movement and served as an original member of “Wake-Up Safe”, a federally certified patient safety organization and was a long-time member and then Chair of the Society for Pediatric Anesthesia Quality and Safety Committee. She also facilitated the development of the original PediCrisis checklists and app, which have subsequently been revised along with a more robust and easier to use app. During her time at Johns Hopkins, she served as the departmental Physician Advisor for Clinical Quality Improvement, was a long-time member and then Chair of the Hospital Risk Management Committee and was a core faculty member of the Armstrong Institute for Patient Safety and Quality. Additionally, her work in cardiac anesthesia was on the leading edge when, in 1990, she led the Transesophageal Echocardiography Program at Johns Hopkins. In 2006, she was one of the founding charter members of the Congenital Cardiac Anesthesia Society. At Children’s National, in addition to her role as Chief, she is currently a member of the Appointment, Promotions and Tenure Committee, oversees the Hospital Pain Committee, and is on the Advisory Board of the Case Western Anesthesiology Assistants Masters Program.
Dr. Heitmiller has mentored many throughout her career and finds her most reward in the successes of her mentees.
 Anita Honkanen, MD
Anita Honkanen, MD
Dr. Anita Honkanen has been at Stanford University since 2003, after spending time in research at the MGH, followed by 4 years in private practice in Florida. As the Chief of Pediatric Anesthesiology and Pain Medicine at Stanford for 13 years, she became committed to developing the careers of her division faculty, mentoring several junior faculty members, fellows, medical and undergraduate students. She has also been a member of Stanford School of Medicine’s Peer Supporter network for several years, now known as Physician Resource Network, providing one-on-one support to fellow physicians with a variety of concerns. She has been advising for WELI since the fall of 2018, and serves on the WELI Steering Committee. Her other interests include work for the AAP, on the Section for Anesthesiology and Pain Medicine, MOCA simulation training, physician-centered creative writing, music, weight lifting, and biking. She is widowed and the mother of five adult daughters (and two small dogs – adopted!).
 Andrew Infosino
Andrew Infosino
Andrew Infosino is a Professor at UCSF in the Department of Anesthesia and Peri-operative Care and the Department of Pediatrics. He did his residency in anesthesiology at UCSF and then his fellowship in pediatric anesthesiology at the Children’s Hospital of Philadelphia. Andrew joined the faculty at UCSF in 1996 and his clinical interests include physiology in infants and children, the pediatric difficult airway, single lung ventilation in infants and children, and emergence delirium. Throughout his career he has been involved in pediatric anesthesia resident and fellow education. For Anesthesia Toolbox, Andrew has created a three-month pediatric anesthesia resident curriculum, is the pediatric anesthesia section editor and is also on their executive board. As the co-chair of the SPA Global Education subcommittee, he responsible for the SPA Global online Lecture Series.
Andrew is actively involved in fellow and junior faculty well-being and professional development and is a strong believer in the need for diversity, especially in leadership positions. He created ViSiPAP in 2017, the Visiting Scholars in Pediatric Anesthesia Program, a reciprocal faculty exchange program, to help “jumpstart” the academic careers of junior faculty and help develop tomorrow’s leaders in pediatric anesthesia. He also developed Fellow/Faculty ViSiPAP, which pairs a fellow with a faculty mentor for local ViSiPAP exchanges, to promote fellow professional development. ViSiPAP is an excellent program for providing women and other UIM faculty with national recognition and opportunities for networking and collaboration. More recently Andrew has encouraged other programs to set up regional ViSiPAP networks.
Andrew is a proud supporter of WELI and has been a WELI advisor since 2019.
 Nathalia Jimenez
Nathalia Jimenez
Dr. Nathalia Jimenez is an Associate Professor in the University of Washington Department of Anesthesiology and Pain Medicine at Seattle Children’s’ Hospital. She is a Clinician Scientist focus on health outcomes in minority children and disparities in health care. Her current research emphasizes the study of social determinants of health, and evaluation of multilevel interventions to improve health outcomes after traumatic brain injury among Hispanic children; work that has been funded by the NIH. She has been privileged to have mentors from different disciplines and believes in the importance of mentoring teams to foster multidisciplinary research and to expand the horizons of academic anesthesia. She feels fortunate to have been trained both in Colombia (South America) and in the United States; which has provided her with opportunities to learn and work with colleagues from different countries. She also serves as Executive Committee member for the School of Medicine Admissions Committee at the University of Washington; Associate member at Harborview Injury Research Center, and the Health Equity Research program at Seattle Children’s Research Institute. Nationally, Dr. Jimenez is the current chair of SPA Diversity Equity and Inclusion Committee and has served for numerous years in the Research Committee. She mentors students from the Schools of Medicine and Public Health, fellows and junior Faculty at the Pediatric Anesthesia Division. She is excited to be part of WELI and see its impact on the future of pediatric anesthesia. On a personal note, she has two adolescent children and is married to an anesthesiologist with whom she balances family and academic life; something that she prioritizes and strives to share with her mentees.
 Dr. Kirk Lalwani, M.B.,B.S., F.R.C.A., M.C.R.
Dr. Kirk Lalwani, M.B.,B.S., F.R.C.A., M.C.R.
Dr. Lalwani completed residency training in Anesthesia and Intensive Care in England at the Norfolk and Norwich University Hospital, King’s College and Royal London Hospitals, followed by a fellowship in Pediatric Anesthesia at Great Ormond Street Hospital in London. After two years as a Visiting Assistant Professor at Seattle Children’s, he moved to Doernbecher Children’s Hospital at Oregon Health and Science University in Portland in 1999, where he is a Professor of Anesthesiology and Pediatrics, Vice-Chair for Faculty Development, and Director of the Pediatric Anesthesiology Fellowship program since its inception in 2002.
Dr. Lalwani has been extensively involved in education and mentorship of medical students, residents, fellows, and faculty for research and career advancement. He was a preceptor for first-year medical students for over 10 years, and is currently serving a second term on the OHSU School of Medicine Admissions Committee. He also serves on the OHSU Faculty Development and Advancement Committee that oversees profesional development across the University. As the current President of the Society for Pediatric Anesthesia, he is passionate about diversity and inclusion in Society activities, engaging under-represented institutions, and global efforts to improve the care of children everywhere through education and research. In his spare time, Dr. Lalwani loves to travel, and is an avid scuba diver, skier, movie buff, and crime fiction afficionado. He spent several years advising teams of neighborhood children for Lego Robotics tournaments, and is excited to be involved with WELI. He is married, and the proud father of two teenaged children.
 Mary Landrigan-Ossar, MD, PhD
Mary Landrigan-Ossar, MD, PhD
Since 2007 my primary clinical focus has been anesthesia for pediatric interventional radiology (IR), taking on the responsibility of Director of IR anesthesia at Boston Children’s Hospital in 2010. There are few pediatric IR suites in the world with as large an anesthesia presence as Boston Children’s where we provide care for more than two thousand cases annually. The breadth of this experience has allowed me to develop a unique area of clinical expertise resulting in peer-reviewed and non-peer-reviewed publications, national and international presentations and participation in pediatric, radiology and anesthesiology policy-making organizations with regard to pediatric interventional radiology.
These activities led to my deeper involvement with vascular anomaly patients. A majority of patients seen in our Vascular Anomalies Center (VAC) have procedures under anesthesia in IR. I have been a member of the VAC since 2010, which, among other responsibilities, involves a weekly multidisciplinary meeting to review patients referred from around the world. This allows for interdisciplinary collaboration at an extraordinarily high level. I have been involved in the description of newly recognized vascular anomalies and in the development of techniques for their diagnosis. I have participated in the working groups that developed management guidelines for these complex syndromes. I have written a chapter on anesthesia for patients with these conditions and have spoken on this topic at grand rounds and at national meetings.
My final major area of clinical and administrative interest is procedural sedation of children. From 2011-2021 I served as chair of the Boston Children’s Hospital Sedation Executive Committee. In this capacity, I was responsible under CMS guidelines for oversight of all procedural sedation performed by non-anesthesiologist practitioners. I have overseen the conversion of all sedation documentation from paper to a consistent electronic format, allowing for seamless oversight and data collection. More recently, I’ve participated in organizing an expansion of the hospitalist sedation service with closer ties to the Department of Anesthesiology, Perioperative and Pain Medicine, paving the way for ongoing improvements in the sedation experience for our young patients regardless of where their sedation is administered. Nationally, I have been a faculty member for the Sedation Provider Course offered by the Society for Pediatric Sedation, and had the privilege of acting as conference organizer for the 2018, 2019 and 2020 annual meetings.
Throughout the sixteen years of my practice at Boston Children’s, I have been enthusiastically active in trainee education. I served as a faculty advisor and member of the Clinical Competency Committee for residents and fellows from 2007-2011. I was chair of the Fellowship Selection Committee from 2011-2015 and had the honor of serving as Associate Program Director for our Pediatric Anesthesia Fellowship, the largest training program in the world for pediatric anesthesiologists, from 2012-2015. I teach residents and fellows in the operating room 40 hours/week and have consistently been evaluated in the top quartile and decile of the faculty by our fellows and residents. I have been the recipient of the Resident Teacher of the Year Award in 2018 and 2020. I have overseen several fellows in the preparation of posters for national presentation or in year-long scholarly projects, and have been the faculty advisor for two students completing their Masters thesis work.
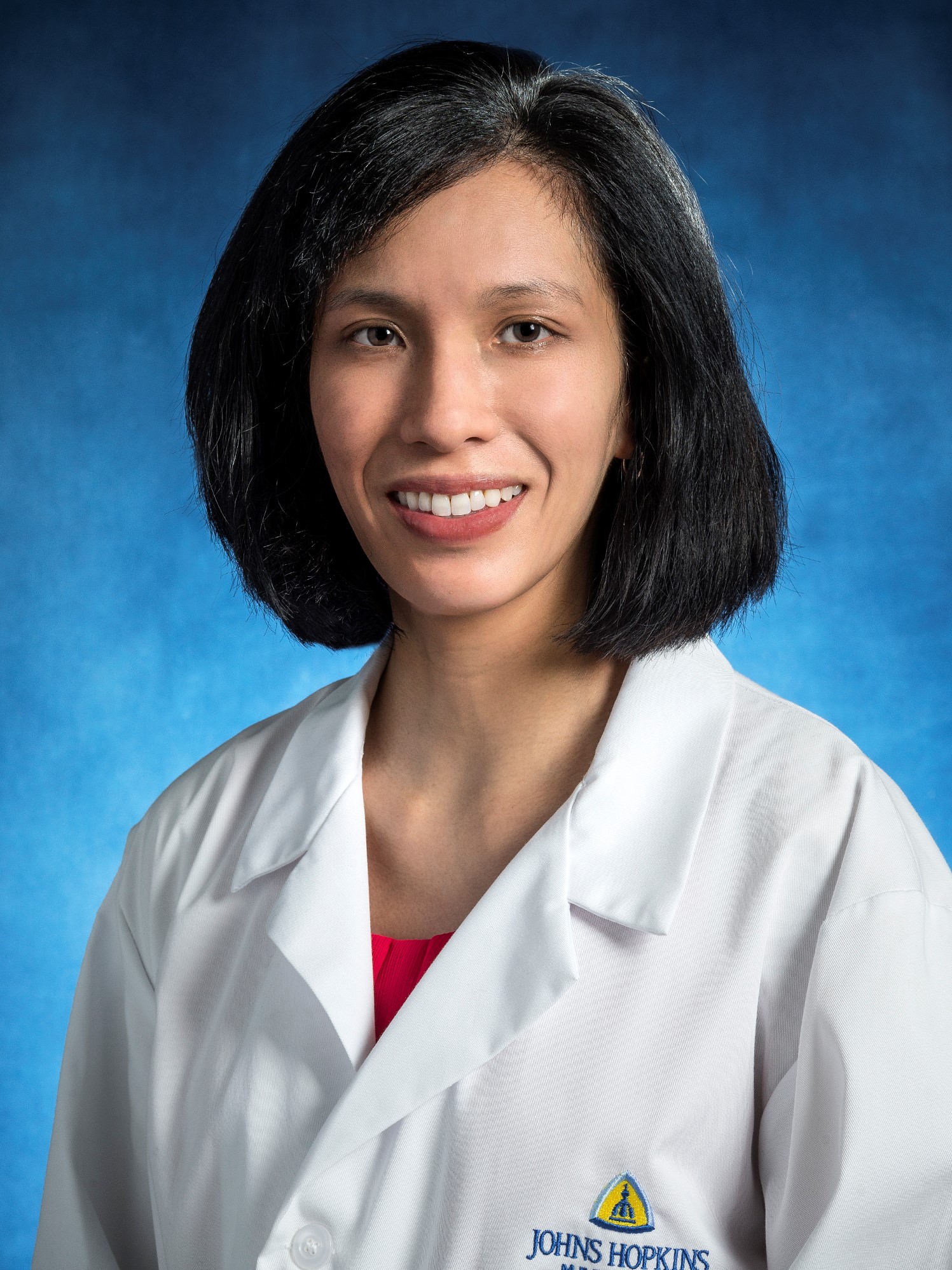 Jennifer K. Lee, MD
Jennifer K. Lee, MD
Dr. Lee is the Founder of WELI and a Professor in the Johns Hopkins Department of Anesthesiology and Critical Care medicine, Division of Pediatric Anesthesiology. She is a clinician-scientist who believes mentoring is one of the most important parts of her job. Jenny has had tremendous mentors and advisors in her life, and she hopes that she can similarly help others. Her research is focused on improving neuroprotection after neonatal and pediatric hypoxic brain injury. She conducts translational research on cerebrovascular blood pressure autoregulation, the effects of hypothermia and rewarming, cell death mechanisms, proteostasis, and white matter injury in clinical and laboratory studies. Her research has been funded by the NIH and several foundations, including the American Heart Association, International Anesthesia Research Society, and the Foundation for Anesthesia Education and Research. Jenny is married to an attorney, and they have two sons.
 Tom Long, MD
Tom Long, MD
 Concetta Lupa, MD
Concetta Lupa, MD
Concetta Lupa, MD, is a Pediatric Anesthesiologist and Professor of Anesthesiology and Pediatrics at the University of North Carolina in Chapel Hill, NC. She completed her anesthesiology residency at the University of North Carolina, and pediatric anesthesia fellowship at Children’s Hospital of Pittsburgh. She has been the pediatric anesthesiology fellowship director at UNC since 2013, and is an active member of the Pediatric Anesthesia Program Director’s Association (PAPDA), where she currently serves as the Secretary/Treasurer and will be the President Elect in May 2020. Additionally, she is the Vice-Chair of the MOCA 2.0 Pediatric Subspecialty Writing Committee. Her professional interests include mentoring junior faculty, residents, and medical students. Clinical and research interests include pediatric colorectal procedures and ERAS pathways, pediatric pain management, and the use of virtual reality for perioperative pain and anxiety management. She recognizes and is greatly appreciative of the amazing formal and informal mentorship that has been bestowed upon her over the years, and is excited to offer guidance to upcoming leaders in pediatric anesthesia.
 Scott Markowitz, MD
Scott Markowitz, MD
Scott Markowitz, MD, is a pediatric anesthesiologist at Children’s Hospital Colorado and an associate professor of anesthesiology at the University of Colorado School of Medicine. Dr. Markowitz has dedicated his academic time extensively to faculty development, working as the director of faculty development in his department, and as an executive leadership advisor, a leadership consultant for teams, and faculty in the Leadership for Innovative Team Science (LITeS) program on the medical campus of the University of Colorado. Dr. Markowitz represents the University of Colorado School of Medicine in the Council of Faculty and Academic Societies (CFAS) of the Association of American Medical Colleges (AAMC). He also collaborates on faculty development and faculty diversity projects with the Dean’s Office in Faculty Affairs. Dr. Markowitz earned his coaching credential from the Weatherhead School of Management at Case Western Reserve University because of the growing evidence of benefit from and desire for advising among healthcare faculty. Dr. Markowitz is also a Gallup-trained Cliftonstrengths Coach and is certified in assessments relevant to leadership development for faculty in healthcare.
 Lynn D. Martin, M.D., M.B.A.
Lynn D. Martin, M.D., M.B.A.
Lynn D. Martin, M.D., M.B.A. is the Medical Director, Continuous Improvement and Innovation at Seattle Children’s. He is a Professor of Anesthesiology and Pediatrics (adjunct) at the University of Washington School of Medicine. He received his M.D. from the University of Washington and his M.B.A. for the University of Tennessee. He completed residencies in both Pediatrics (Phoenix Children’s Hospital) and Anesthesiology (Johns Hopkins University) followed by fellowships in pediatric anesthesiology and pediatric critical care medicine at Johns Hopkins University. He is board certified by the American Board of Anesthesiology with specialty certification in pediatric anesthesia and the American Board of Pediatrics with specialty certification in pediatric critical care medicine. Dr. Martin has served as the president of the Society for Pediatric Anesthesia. His original research interests involved conventional and non-conventional forms of mechanical ventilation and more recently focus on quality improvement, patient safety, and operative outcomes research.
 John J. McAuliffe, MD, MBA
John J. McAuliffe, MD, MBA
Dr. McAuliffe began his career at CCHMC in 1985 in the Department of Anesthesia. Over the years he has taken on increasing responsibilities in the department. By 1994 he was named associate director. From 2002-2014 he served as research director. From 2008-2016, he added the role of director of the Division of Neurobiology. He was named section chief of Intraoperative Neurophysiological Monitoring in 2010. In 2016 he was named Interim Chair of the Department of Anesthesia and was appointed to the position of Anesthesiologist-in-Chief in February of 2017. Dr. McAuliffe served on the board of the American Society of Neurophysiological Monitoring from 2012-2016 and was President of this organization from 2014-2015. He is a member of the Pediatric Anesthesia Leadership Council and has recently been appointed as a mentor for the Women’s Empowerment and Leadership Initiative within the Society for Pediatric Anesthesia. His current interests include leadership development and applications of AI and machine learning to improve patient care.
 Asha Padmanabhan, MD, FASA
Asha Padmanabhan, MD, FASA
Asha Padmanabhan, MD, FASA is Board Certified in Anesthesiology and Pediatric Anesthesiology. After obtaining her Medical Degree in India, she moved to the UK for several years where she trained in Anesthesiology. She followed that with a Residency in Anesthesiology at the Beth Israel Deaconess Medical Center, Harvard University, in Boston. After a brief 3 year stint in Academic Medicine at the Johns Hopkins Bayview medical Center in Baltimore, she moved to Private Practice in sunny Florida. From being the Treasurer and Managing Partner of her Private Practice group, to Chief of Anesthesia at a Community hospital with a large group practice Envision Physicians, to now being Medical Director of Anesthesia at Bethesda West Hospital, she has held several leadership positions. Wanting to make a difference, she joined the Florida Society of Anesthesiologists and was elected to the Executive Board 2 years ago and now holds the position of Treasurer. She has also actively advocated for women physicians at the American Society of Anesthesiologists and is currently Vice Chair of the Committee on Women Anesthesiologists. Having been in leadership positions for over 10 years, she realized early on that women physicians in leadership or aspiring to be leaders face a unique set of challenges. As an ‘accidental leader’ being thrown into leadership totally unprepared, she soon realized how lonely and isolating being a woman physician in leadership was, and the lack of resources available. Having been through several leadership training programs over the years, she became passionate about sharing what she learned through her own leadership struggles with other women physicians by creating networking groups and mentoring and advising women physicians. She has run workshops and mentored young women physicians through her local and state medical societies. Flirting with the edges of burnout, she explored coaching as a way to enhance her own leadership skills and find more fulfillment in medicine. Being coached helped her realize Coaching was the very foundation to building skills to achieve career fulfillment and be a resilient leader. Her own personal transformation through Coaching into being a happier human being, a more effective leader, mentor and sponsor encouraged her to train as a Physician Coach. She coaches women physicians in Leadership Development, Career Transformation, and Career Resilience. She loves working with women physicians in early career looking to find ways to balance career ambitions with family life, as well as mid-career physicians looking for a career pivot or looking for fulfillment and a renewed sense of passion in their careers. Her goal is to empower women physicians to be the leaders they are meant to be, at work and at home, even without a formal leadership title
 Dr. Peggy McNaull
Dr. Peggy McNaull
Peggy McNaull currently serves as the Associate Chief Medical Officer for Quality and Safety for UNC Medical Center, the interim Director for Quality for UNC Faculty Practice, and the Vice Chair of Patient Safety and Quality Improvement for the Department of Anesthesiology. She attended medical school at Louisiana State University School of Medicine, completed her residency in Anesthesiology and fellowship in Pediatric Anesthesiology at UNC, and then completed her fellowship in Pediatric Cardiovascular Anesthesia at Texas Children’s Hospital. Dr. McNaull is committed to advancing the UNC Healthcare mission of promoting high quality, high value care to our patients across the state of North Carolina. The quality efforts that bring her the most joy include Opioid Stewardship and Enhanced Recovery After Surgery.
Dr. McNaull is very involved in advancing the field of Anesthesiology, specifically the specialty of Pediatric Anesthesiology. She holds leadership positions with both the American Board of Anesthesiology and the Society for Pediatric Anesthesia.
 Sara Pittenger, MD
Sara Pittenger, MD
Sara Pittenger, MD, is an Associate Professor of Anesthesia and Pediatrics at the University of North Carolina in Chapel Hill, NC. She currently serves as the Division Chief of Pediatric Anesthesiology and the Medical Director of the Pediatric Sedation service. She completed her M.D. at Northwestern University in Chicago and earned both her anesthesiology residency and pediatric anesthesiology fellowship at the University of Chicago. Since joining the UNC faculty in 2010, she has been actively involved in medical student, resident, and fellow education and mentorship. She serves as a medical student career goals advisor and has mentored both MD and MPH student on various quality improvement projects focused on improving pediatric perioperative care. Dr. Pittenger is committed to leading quality improvement processes at NC Children’s Hospital in her role as Co-Director of the UNC Children’s Improvement Council. Her clinical interests and focus include congenital cardiac anesthesia and pediatric procedural and imaging sedation. In her free time, Dr. Pittenger enjoys spending time with her husband and two children cooking, gardening, and being outdoors.
 Jennifer Rabbitts, MD
Jennifer Rabbitts, MD
Dr. Jennifer Rabbitts is an Associate Professor of Anesthesiology and Pain Medicine at the University of Washington School of Medicine. She practices as a pediatric anesthesiologist and pain physician at Seattle Children’s Hospital. Her NIH-funded research program focuses on assessing and improving pain and health outcomes after pediatric surgery. She is specifically interested in bio-psychosocial risk and resilience factors for delayed recovery, mechanisms underlying acute to chronic pain transition and treatments to enhance recovery and improve long-term pain and health outcomes in adolescents undergoing major surgery. Dr. Rabbitts is active in service, currently serving on the scientific program committee for the International Symposium of Pediatric Pain, and on the editorial boards of the Journal of Pain, and Pediatric Anesthesia. She is passionate about mentoring students and early career faculty, and founded an early career development group for faculty on K awards at her institution, and lead the Early Career Forum at the American Pain Society for several years. Dr. Rabbitts and her husband, who is also a physician scientist, enjoy spending time in the Pacific Northwest outdoors with their two young boys.
 Srijaya Reddy, MD, MBA
Srijaya Reddy, MD, MBA
Srijaya Reddy is an Associate Professor of Anesthesiology at Monroe Carell Jr. Children’s Hospital at Vanderbilt University Medical Center. She completed her anesthesiology residency at Henry Ford Health System in Detroit, Michigan, and pediatric anesthesiology fellowship at Children’s National in Washington, District of Columbia. She also received her MBA in Healthcare from the George Washington University School of Business. Dr. Reddy provides perioperative anesthesia care for infants and children, with a focus on children undergoing craniofacial surgery, neurosurgical procedures, and liver transplant. She is an Associate Editor for the Journal of Education in Perioperative Medicine (JEPM), an Executive Committee member for the Pediatric Craniofacial Collaborative Group (PCCG), and an ABA Oral Board Examiner. Dr. Reddy enjoys working with and mentoring residents, fellows, and junior faculty, and finds it rewarding watching her mentees succeed in their endeavors. She has been involved with WELI since the spring of 2019 and is enthusiastic about being a part of this important initiative. She has one son, Kethan, who her greatest reward.
 Lori Q. Riegger, MD
Lori Q. Riegger, MD
Lori Riegger is an Associate Professor of Anesthesiology at Michigan Medicine in Ann Arbor, where she has been on faculty since 1993. She also completed her residency and fellowship at the University of Michigan. She has been the chief of the Congenital Cardiac Anesthesia Team since 2000 and her academic interests—clinical, research, educational and administrative—all revolve around improving the care of patients with congenital heart disease. After a fabulous and focused year as a mentee in WELI during its first year, she has recognized what a treasure an outstanding mentor is. She is committed to try to follow in the footsteps of her wonderful mentor, as a WELI mentor/advisor. For fun she loves to hang out with her family, walk her dog, be outside, and go mountain hiking via ferrata.
 Dr. Patrick Ross
Dr. Patrick Ross
Dr. Patrick Ross is a pediatric intensivist and anesthesiologist in the Department of Anesthesiology Critical Care Medicine at Children’s Hospital Los Angeles. His current academic rank is Associate Professor of Anesthesiology and Pediatrics at the Keck School of Medicine of the University of Southern California. He completed training and is board certified in pediatrics (Lucile Packard Children’s Hospital), pediatric critical care (UCSF), anesthesiology (UCSF) and pediatric anesthesiology (Children’s Hospital of Philadelphia). Dr. Ross is a member of his Department’s Research Oversight Committee and was previously the Program Director for CHLA’s Pediatric Critical Care Medicine Fellowship for five years. He used these opportunities to conduct research primarily in the area of respiratory physiology. Dr. Ross is currently the Medical Director for Respiratory Care at Children’s Hospital Los Angeles.
 Jamie M. Schwartz, MD
Jamie M. Schwartz, MD
Dr. McElrath Schwartz is Co-Chair of WELI and an Assistant Professor in the Johns Hopkins Department of Anesthesiology and Critical Care Medicine. Her clinical practice includes both pediatric critical care and anesthesia, with emphasis on patients with cardiac disease. She is a program builder who values people and teamwork. In her role as Division Chief of Pediatric Critical Care Medicine and Director of the Pediatric Critical Care Unit, she works with a large team of faculty and staff to develop and maintain the system required to care for children with critical illness. She was recently named Co-Director of the Blalock Taussig Thomas Pediatric and Congenital Heart Center at Johns Hopkins where she oversees an interdepartmental system that cares for children with cardiac disease from birth to adulthood. To succeed in these roles, she utilizes an approach that intentionally brings leadership and business principles into the clinical arena. She has benefitted from the trailblazing of great women leaders before her and formal mentorship and business advising. WELI has provided an avenue for Dr. Schwartz to share her excitement about women’s leadership through program building, advising, networking and shared growth. WELI also gives her tools to that she uses in her other job, parenting her two children, Taryn, age 14 and Max, age 11.
 Paul Stricker, MD
Paul Stricker, MD
Paul Stricker, MD is an Associate Professor and the Associate Chief for Research in the General Anesthesiology Division at the Children’s Hospital of Philadelphia. He is a graduate of the Intermountain Advanced Training Program in Healthcare Delivery Improvement at Intermountain Healthcare, Salt Lake City, Utah.
Dr. Stricker is a clinical outcomes researcher whose focus has included clinical outcomes research using observational databases in children undergoing complex cranial vault reconstruction surgery. In 2012 Dr. Stricker worked with SPA members to found the Pediatric Craniofacial Collaborative Group, an international consortium of pediatric clinical researchers from over 30 institutions and three countries. He has led this group in creating the multicenter Pediatric Craniofacial Surgery Perioperative Registry, and has subsequently led the publication of multiple scientific articles with this group.
Dr. Stricker is a Senior Scholar at the Penn Center for Perioperative Outcomes Research and Transformation (CPORT). He leads the Pedi-INQUIRE research group at the Children’s Hospital of Philadelphia, whose mission is to determine pediatric clinical perioperative outcomes using bioinformatics, scientific, and quality improvement methodologies, and to develop interventions to improve them.
In 2016 Dr. Stricker founded and currently leads the Pediatric Perioperative Outcomes Group, an international collaboration whose mission is to develop core outcome sets for pediatric perioperative research, thereby promoting the integration of patient-centered outcomes in clinical research. This group’s membership includes investigators from eleven countries on six continents, and counts among its members thought leaders in the specialty.
 Kim Strupp, MD
Kim Strupp, MD
Dr. Kim Strupp is a pediatric anesthesiologist at Children’s Hospital Colorado and an Associate Professor of Anesthesiology at the University of Colorado. She completed her medical training at the University of Wisconsin School of Medicine and Public Health followed by residency and Pediatric Anesthesia fellowship at the Mayo Clinic in Rochester, Minnesota. She currently serves as the Director of Performance Improvement in the Pediatric Anesthesiology Section and she is passionate about patient safety and quality improvement. Dr. Strupp is also the Associate Program Director for the 2nd year fellowship in Quality Improvement. She serves as an attending on the Acute Pain Service and has expertise in pediatric regional anesthesia. Dr. Strupp has been a WELI mentee herself since the inception of the program, and she is excited for the opportunity to share her time and experiences as a mentor in the program. She is an active member of the SPA’s Quality and Safety Committee, as well as the Critical Events Checklist Subcommittee. Dr. Strupp and her husband enjoy spending time with their two young children in the Rocky Mountains!
 Judit Szolnoki, MD, MS PSL
Judit Szolnoki, MD, MS PSL
Dr. Judit Szolnoki is a pediatric anesthesiologist practicing at Nemours Children’s Hospital in Orlando, Florida where she is chair of the Department of Anesthesiology. In addition, Dr. Szolnoki is on faculty for the Clinical Quality, Safety and Leadership Master’s program at Georgetown University.
Dr. Szolnoki is a native of Hungary, received her medical degree from Semmelweis University Medical School, Budapest, Hungary. She completed her residency in anesthesiology in Syracuse, NY and pediatric fellowship at Children’s Hospital Colorado.
Dr. Szolnoki has a master’s degree in Patient Safety Leadership and a coaching certificate from Erickson Coaching International. She believes in servant leadership and the power of mentorship, sponsorship and coaching in the development of young faculty. Dr. Szolnoki has special interest in managing difficult pediatric airways and providing peer support to “second victims”. Judit is married to her husband, Ferenc and has three (mostly) grown children (and a small zoo: two dogs, a cat, two grand-kittens. Not even counting the gopher turtle that took habitat in my back yard, plus the deer, the possum, the sandhill cranes who visit on a regular basis).
 Jonathan M. Tan, MD MPH MBI FASA
Jonathan M. Tan, MD MPH MBI FASA
Jonathan M. Tan, MD MPH MBI FASA is an Assistant Professor of Anesthesiology and Spatial Sciences at the Children’s Hospital Los Angeles (CHLA), the Keck School of Medicine, and the Spatial Sciences Institute at the University of Southern California. He is board certified in Anesthesiology, Pediatric Anesthesiology, Clinical Informatics and Medical Quality. He was a Joseph E. Robert Jr. Fellow in Pediatric Surgical Innovation at the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National. Prior to arriving at CHLA, Dr. Tan has had the privilege of practicing in some of the top children’s hospitals including, the Children’s Hospital of Philadelphia (CHOP), the Children’s Hospital of Pittsburgh, and Children’s National. In his most recent appointment at CHOP, Dr. Tan held a secondary appointment in the Department of Biomedical and Health Informatics, was a Senior Fellow at the Leonard Davis Institute for Health Economics at the University of Pennsylvania, Senior Fellow at the Penn Center for Public Health, and Senior Scholar at the Penn Center for Perioperative Outcomes and Research Transformation. He has been invited to speak nationally and internationally at anesthesiology, data science, informatics, spatial science, medical geography, patient safety and quality improvement, pediatric surgery, and public health conferences. Dr. Tan currently serves on the American Society of Anesthesiologists Committee on Informatics and Information Technology, the Anesthesia Patient Safety Foundation (APSF) Committee on Technology, the APSF Patient Safety Advisory Committee on Clinical Deterioration and the Committee on Infectious Diseases. Dr. Tan’s work focuses on developing data science methods to understand the impact of where a patient lives and social determinant of health risk factors on pediatric patient safety and health outcomes. He has grant funding from the Anesthesia Patient Safety Foundation (APSF) and Foundation for Anesthesia Education and Research (FAER) to study “The Impact of Air Quality and Neighborhood-Level Risk Factors on Pediatric Perioperative Respiratory Adverse Events.” Using spatial analysis, Dr. Tan is building a platform to improve the way we risk stratify, communicate, and care for pediatric patients.
Areas of expertise to mentor in: Clinical Informatics, Social Determinants of Health, Spatial Data Science, Health Economics, Quality Improvement in Pediatric Anesthesiology
 Amy Vinson
Amy Vinson
Amy Vinson is a Pediatrician and Pediatric Anesthesiologist at Boston Children’s Hospital and is an Assistant Professor of Anesthesia at Harvard Medical School. She attended college and medical school in Georgia before coming to New England where she completed a residency in pediatrics at Brown, an anesthesiology residency at BIDMC and Pediatric Anesthesiology fellowship at Boston Children’s Hospital, where she served as chief fellow. She has a long standing interest in wellness, burnout, peer support, and substance use disorder in anesthesiologists and has lectured widely on these subjects. She established wellness programs at Beth Israel Deaconess Medical Center and Boston Children’s Hospital and has consulted on the formation of many other programs throughout the country. She currently serves as the Chair of the ASA’s Committee on Physician Well-being, is the ASA representative to the National Academy of Medicine’s Clinician Well-being Collaborative, and is the Director of Clinician Well-being in her own department. Her research on Burnout in Anesthesiologists – the largest such study of anesthesiologists to date, has just been published in Anesthesiology and she has numerous other publications and research manuscripts on subjects related to overall physician well-being. She is a self-described “well-being pragmatist” focusing on systemic and organizational factors impacting well-being and burnout. To stay balanced, she enjoys time with family, making music, fitness and home improvement projects.
 Emmett Whitaker
Emmett Whitaker
Dr. Emmett Whitaker is Associate Professor of Anesthesiology, Neurological Sciences, and Pediatrics at the University of Vermont Larner College of Medicine. Dr. Whitaker completed his medical education at the University of Rochester School of Medicine and Dentistry and his anesthesiology residency and fellowship at Johns Hopkins Hospital. After training, he spent 5 years as an attending pediatric anesthesiologist at Nationwide Children’s Hospital where he and his colleagues developed an infant spinal anesthesia from the ground up. The anesthesia group at NCH has performed more than 1000 spinal anesthetics since 2015. Currently, Dr. Whitaker splits his time between clinical anesthesia practice and translational science. His lab studies the effects of early-life insults on the development of the brain and cerebral vasculature. Recently, he was awarded a Foundation for Anesthesia Education & Research Mentored Research Training Grant during which he will study the effects of sevoflurane on cerebrovascular autoregulation in neonatal offspring of preeclamptic pregnancies. Dr. Whitaker is passionate about mentorship and sponsorship of women in medicine, particularly as it pertains to early career women who are interested in academics. He has a strong track records of mentoring undergraduates, medical students, residents, fellows, and junior faculty. One of his proudest professional achievements was being the Program Chair for the Society for Pediatric Anesthesia 2021 Annual Meeting, “A Celebration of Women in Pediatric Anesthesiology”, for which greater than 80% of speakers and moderators were women. Dr. Whitaker lives in rural Vermont with his husband Andrew and his two dogs, Charlie and Bernie.
 Gina Whitney
Gina Whitney
I am currently at the Children’s Hospital Colorado where I have been since January 2015. I am a cardiac anesthesiologist who also serves our group as the Associate Chief of Pediatric Anesthesiology. My primary interest is in Clinical Quality Improvement and Patient Safety, and I serve as the Medical Director for Children’s Anesthesia for the American College of Surgeons Children’s Surgery Verification Program at CHCO. I did my training initially in Pediatric Intensive Care and Cardiac Intensive Care at UT Southwestern and Texas Children’s Hospital. I joined the Pediatric ICU faculty at Vanderbilt University after I completed my first round of training where I developed a strong interest in clinical quality and safety. I completed the Improvement Advisor Program through the Institute for Healthcare Improvement in Boston, MA. I went back to complete training in Anesthesiology and Pediatric Anesthesiology at Vanderbilt. I made the move to sunny Colorado in 2015 where I have enjoyed practicing congenital cardiac anesthesiology and helping to further develop clinical quality and safety programs. I serve as a coach for the CU School of Medicine’s Institute for Healthcare Quality Improvement and am in the midst of completing an MBA in Healthcare Administration. (I have promised my mother that I am done with school after this one last bit of training. I am so excited to see the growth of the WELI program – such a great resource for all of us in the practice of pediatric anesthesiology.
 Julie Williamson, DO
Julie Williamson, DO
I trained in general pediatrics at the University of Maryland, followed by anesthesiology residency and pediatric anesthesiology and critical care fellowships at Johns Hopkins School of Medicine. I was a formal mentor to medical students at the Stanford School of Medicine, and have served as the Anesthesiology Program Director at Emory since 2016. The highlight of the position is helping my residents and fellows construct their own goals and career pathways and mentoring them to achieve what they have designed. I enjoy the clinical practice of both anesthesiology and critical care, especially trauma resuscitation and complex airway management. My husband Dan and I have a teenaged son and a tweenaged daughter.
Anita Akbar Ali
Dean Andropoulos
Sean Barnes
Stephanie Black
James Bradley
Elizabeth Brill
David Buck
Christina Diaz
Faye Evans
Sean Flack
Nancy Glass
Cheryl Gooden
Nina Guzzetta
Doris Hardacker
Stephen Hays
Ranu Jain
Jeff Koh
Elliot Krane
Anjana Kundu
Tom Long
Lynn Maxwell
John McCloskey
Frank McGowan
Wanda Miller-Hance
Bukky Nafiu
Viviane Nasr
Toyin Olutoye
Christine Park
Jerry Parness
Sophie Pestieau
Dan Roke
Allison Ross
Senthil Sadhasivan
Larry Schwartz
Deb Schwengel
Hal Shaffner
Sol Soriano
Rosalie Tassone
Joe Tobin
Sam Wald
Eric Wittkugel
Sam Yanofsky
Myron Yaster
 Click Here for Registration
Click Here for Registration WELI members have the ability to search through our databank of topics and speakers with areas of expertise from national talks.
WELI members have the ability to search through our databank of topics and speakers with areas of expertise from national talks. Use the Society for Pediatric Anesthesia’s job bank to explore current open positions all around the country in the field of anesthesiology.
Use the Society for Pediatric Anesthesia’s job bank to explore current open positions all around the country in the field of anesthesiology. Supported By The Society for Pediatric Anesthesia
Supported By The Society for Pediatric Anesthesia